
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 2025-02-26
Date: 25-2-2016
Date: 2025-03-22
|
Diabetes Mellitus
The definition, classification, epidemiology, pathogenesis, morphology, clinical features, diagnostic criteria, & complications of diabetes mellitus will be discussed next in this sequence.
1. Definition
DM represents a heterogeneous group of disorders that have hyperglycemia as a common feature.
It can also be defined as a chronic metabolic abnormality of CHO, Fat, and Protein.
2. Classification
Although all forms of DM are characterized by hyperglycemia the pathogenic mechanism by which hyperglycemia arises differ widely.
Recent classification of DM is based on the pathogenic mechanism that led to the development of the diabetic syndrome rather than age of onset and type of therapy. As to the new classification there are four types of diabetes of which the first two are the major types.
A. Type 1 DM
further classified as type1A and type1B.
• Type 1A DM results from autoimmune beta cell destruction which results in absolute insulin deficiency
• Type 1B (idiopathic group) is also characterized by insulin deficiency and a tendency to develop ketosis. The cause that led to insulin deficiency is not known
B. Type 2 DM
• It is a heterogeneous group of disorders usually characterized by variable degrees of insulin resistance, impaired insulin secretion, and increased glucose production.
C. Other specific types of DM
Other causes for DM include specific genetic defects in insulin secretion or action, metabolic abnormalities that impair insulin secretion, conditions that impair glucose tolerance, exocrine disease of the pancreas that lead to destruction of beta cell, several endocrinopathies that can lead to DM as a result of excessive secretion of hormones that antagonize the action of insulin.
D. Gestational diabetes
N.B- the previously used terms, NIDDM to represent type 2 DM and IDDM to represent type 1 DM, are obsolete.
3. Epidemiology
• The prevalence of DM has increased dramatically in the world due to the increasing urbanization and consequent life style changes.
• There is considerable variation in DM prevalence among different ethnic groups world wide due to both genetic and environmental factors.
• Type 2DM accounts to 80% of all cases and type 1DM accounts to 5-10% of all cases of diabetes.
• The incidence of DM is similar in men and women throughout most age ranges but is slightly greater in men> 60 years of age.
4. Pathogenesis
A. Type 1A DM
• there is an autoimmune destruction of beta cells of the pancreas
• It is at least after 80% of the beta cells are destroyed that a metabolic
abnormality appears in IDDM.
• The pathogenesis begins with a genetic susceptibility and some environmental factors initiates the autoimmune process in such susceptible individuals.
Genetic factors/ evidences
1. Less than 20% of Type 1 diabetics have a parent or sibling with the disease. This can be sited as evidence that genetic factors are involved in the pathogenesis of the disease.
2. In studies of identical (monozygotic) twins in which one or both were diabetic, both members of the pair were affected in approximately half of the cases [i.e. there is a 50% concordance rate]
• N.B these 50 % concordance rate shows that environmental factors contribute to the development of the disease on a heritable predisposition
3. Type 1 DM is believed to be a polygenic disorder. Additional evidence came from studies of genes that code for antigens of the major Histocompatibility complex. In patients with type 1 diabetes, 95% express either HLA- DR3 or HLA – DR4, or both, compared with 40% of the general population who exhibit the above MHC genes.
The above three genetic factors/ evidences show that there is a genetic factor that is/ are important for the susceptibly to the disease and environmental factors are required to the development of an autoimmune reaction on these susceptible individuals.
Autoimmunity
- This is a development of auto antibodies to self-antigens.
- Environmental factors are essential for the development of the autoimmune process but the exact mode of their action is not clear (see the proposed mode of action below in the discussion of environmental factors).
- Evidences for autoimmune involvement in the destruction of B cells towards the development of Type 1A DM are as follows.
1. Circulating auto- antibodies against components of the beta cells and against insulin were demonstrated in the large majority of all newly diagnosed children with diabetes.
2. The destruction of beta cells by an immune response is also evidenced by the presence of mononuclear cell infiltrates in the pancreatic tissue of a patient with type 1 diabetes .
Environmental factors
As mentioned earlier, the fact that a significant proportion of monozygotic twins remain discordant for Diabetes suggests that non-genetic factors are required for development of diabetes.
- The environmental factor in many cases that is responsible for the initiative of an autoimmune reaction is believed to be a viral infection of the pancreas.
- Coxsakievirus, Rubella virus, Infectious mononucleosis, Mumps and other viruses are incremented as viral causes
- Presumably, viral infections of the pancreas could induce diabetes by two mechanisms.
Direct inflammatory disruption of islets( which is a rare cause of DM) or induction of an autoimmune response by exposing crypting B cell antigens.
- It has also been suggested that exposure to proteins contained in cow's milk may be an environmental trigger for type1 diabetes. This is because milk proteins provide specific peptides that share antigenic sites (molecular mimicry) with human B cell surface proteins there by eliciting the production of auto reactive antibodies.
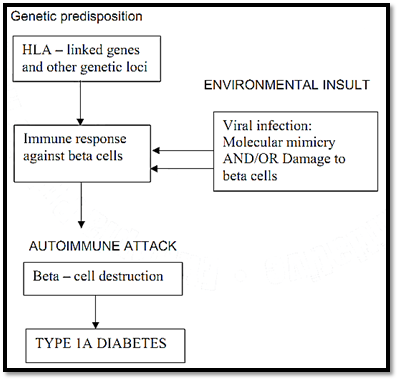
Figure -1- Suggested pathogenic mechanism of type I DM
B. Type 2 DM
Pathogenesis
• Is also a polygenic disorder
• Central to the development of type 2 DM are insulin resistance and abnormal insulin secretion. Many believe that peripheral insulin resistance precedes the latter
Genetic factors
• 60% of patients have either a parent or sibling with this disease
• >80% concordance rate in monozygotic twins
• The above figures suggests that type 2 DM has strong genetic basis than type 1 DM
• No association with MHC class genes is found
• Despite the defect in insulin secretion, many patients with type 2 diabetes have increased insulin concentration in the blood in an attempt to overcome the peripheral insulin resistance. The hyperinsulinemia in turn results in decreased insulin receptors peripherally in the muscle and adipose tissue.
Environmental factor
The major environmental factor is obesity, which augments the genetically determined insulin resistance of type 2 DM
Pathophysiology
Type 2 DM is characterized by three pathophysiologic abnormalities: impaired insulin secretion, peripheral insulin resistance, and excessive hepatic glucose production.
Insulin resistance.
- Is a prominent feature of type 2 DM
- Is caused by decreased efficiency of insulin to act on peripheral tissue especially liver and skeletal muscles.
- The precise mechanism of insulin resistance is unknown but a post receptor defect is believed to play the major role.
- Insulin resistance leads to:
A. Decreased peripheral utilization of glucose. So increased blood glucose
B. Increased hepatic glucose production
Impaired insulin secretion
- The reason for the impairment of insulin secretion is not clear
- Genetic defect, increased hyperglycemia (“glucose” toxicity), increased free fatty acid level (“lipotoxicity”)- all are suggested as a cause or factors which worsen beta cell failure to secrete insulin Increased hepatic glucose production
- Insulin promotes storage of glucose as hepatic glycogen and suppresses gluconeogenesis.
- Unopposed action of insulin counter regulatory hormones results in increased hepatic glucose production.
5. Pathology (Morphology)
Type 1
• The characteristic lesions in the pancreases of children, who suffer from type1 DM, predominant lymphocytes infiltration, are seen in the islets accompanied by few
macrophages. The B cell mass is significantly decreased.
Type 2
• No decrease is the number of beta cells and there is no morphologic lesion of these cells.
• Amyloid deposition is seen specially in patients older than 60 years of age In some patients fibrosis of the islets is also seen
6. Clinical manifestations
• Symptoms are due to hyperglycemia
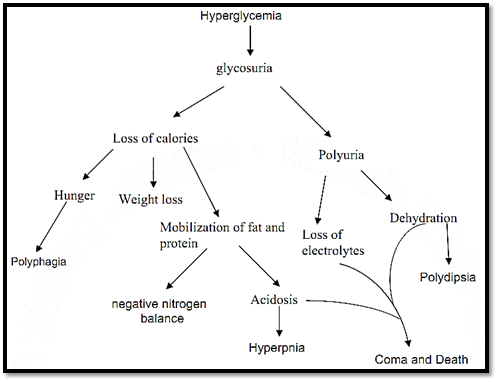
Figure -2- The clinical consequense and complication of DM
• Patients may present with classical symptoms of diabetes
Polyuria, polydipsia, polyphagia with weight loss or they may present with DKA.
7. Diagnosis
Is based on the criteria set by Consensus panels of experts from the National Diabetes Data Group
• Symptoms of DM plus random blood glucose concentration of > 200mg/dl Or
• Fasting plasma glucose > 126mg/dl. Or
• Two hour plasma glucose > 200mg/dl during an oral glucose test (i.e. after an oral dose of 75g glucose dissolved in water)
*In the absence of unequivocal hyperglycemic and acute metabolic decompensation, these criteria should be confirmed by repeat testing on a different day.
8. Complications of Diabetes
A. Acute complications
i. Hypoglycemia
Common in Type1 patients.
Causes:
May be caused by missing meals or doing unexpected exercise after taking insulin doses. In diabetic patients with autonomic neuropathy, there could be hypoglycemic unawareness. This is so because the patient doesn’t have symptoms of hypoglycemia, and won’t take appropriate measure.
Symptoms:
Symptoms of hypoglycemia include sweating, nervousness, tremor, and hunger if it is not corrected in time central nervous system symptoms ensue like confusion, abnormal loss of consciousness or convulsions.
ii. Diabetic ketoacidosis.
Mostly a complication of Type1DM
• Insulin deficiency coupled with Glucagon excess results in Accelerated ketogenesis (ketone body production) ------ DKA.
• Insulin deficiency results in activated lipolysis and so increased free fatty acid concentration in the plasma
• As a result body fat is metabolized as a source of energy. This oxidation produces ketone bodies (acetoacetic acid and Beta hydroxybutyric acid), which are released into the blood and lead to metabolic acidosis.
• Inadequate levels of plasma insulin for a variety of reasons can precipitate DKA. See the list below
Precipitating events:
Inadequate insulin administration
Infection (pneumonia/UTI/gastroenteritis/sepsis … etc.)
Infarction (cerebral, coronary, mesenteric)
Drugs
• Clinically, ketoacidosis begins with anorexia, nausea and vomiting , coupled with Polyuria . If condition is not treated it may go into altered consciousness and coma.
iii. Non-ketotic Hyperosmolar state
• Is usually a complication of Type 2 because there is enough insulin to prevent ketosis
• Patient present with profound dehydration resulting from a sustained hyperglycemic diuresis and finally goes to a comatose state
B. Late complications of Diabetes
Mechanisms of development of diabetic late complications:
Long-term hyperglycemia is essential for the development of diabetic late complications. Many mechanisms linking hyperglycemia to the complications of long-standing diabetes have been explored. Currently two such mechanisms are important.
1. Non-enzymatic glycosylation.
• Non-enzymatic binding of glucose (glycosylation) to cellular proteins. This leads to formation of advanced glycosylation End product (AGEs) which cross link proteins (e.g.. collagen, extra cellular proteins), promote glomerular dysfunctions, induce endothelial dysfunctions, and alter extra cellular matrix composition and structure.
• AGEs have been shown to accelerate atherosclerosis.
Increased Glycosylated low-density lipoproteins (LDL), which do not readily bind to the LDL receptor in the liver, thereby making LDL cholesterol available to the arterial wall.
2. Hyperglycemia leads to increased intracellular glucose, which is then metabolized by aldose reductase to sorbitol, a polyol, and eventually to fructose. These changes have several untoward effects. The accumulated sorbitol and fructose lead to increased intracellular osmolarity and influx of water, and eventually, to osmotic cell injury. In the lens, osmotically imbibed water causes swelling and opacity ------- cataract formation. Sorbitol accumulation also impairs ion pumps and is believed to promote injury of Schwann cells and pericytes of retinal capillaries, with resultant peripheral neuropathy and retinal microaneurysms.
Diabetic macro vascular disease:
• Atherosclerosis
> The extent and severity of atherosclerotic lesions in large and medium sized arteries are increased in long standing diabetes, and their development tends to be accelerated.
Atherosclerotic lesions in large blood vessels lead to vascular insufficiency and an ultimate production of ischemia in the organs supplied by the injured vessels. E.g. Myocardial infarction, Brain infarction (resulting in stroke), gangrene of the toes and feet.
Diabetic micro vascular disease
Increased thickening of the basement membrane in small vessels leads to the following chronic complication:
Diabetic Retinopathy
- DM is the leading cause of blindness in the developed world at ages>20.
- Blindness is primarily the result of progressive diabetic retinopathy and significant macular edema
It is classified into two
1. Non – proliferative retinopathy
• Is characterized by retinal vascular micro aneurysms, blot hemorrhages, and cotton wool spots
2. Proliferative retinopathy
• As the vascular abnormalities tends to be severe, new blood vessels start to proliferate in the retina
Diabetic Nephropathy
• It is the leading cause of ESRD (End stage renal disease) in the developed world.
• It starts with microalbuminuria (30-300 mg/d in a 24 hr urine collection) and progresses to overt proteinuria (> 300mg/d) Three important lesions are in a patient with diabetic nephropathy.
Thickening of glomerular basement membrane which results in glumerulosclerosis, renal arteriosclerosis as part of the systemic Involvement of blood vessels, and pylonehphritis.
Diabetic Neuropathy
- It occurs in approximately 50% of individuals with DM
- It may manifest as polyneuropathy, mononeuropathy, and /or autonomic neuropathy
a. Polyneuropathy
- The most common form of diabetic neuropathy is distal symmetric polyneuropathy. It most frequently presents with distal sensory loss, Hyperesthesia, paraesthesia and pain also occur.
b. Mononeuropathy
- This is less common than polyneuropathy in DM and presents with pain and motor weakness in the distribution of a single nerve.
- Involvement of 3rd
cranial nerve is most common sometimes-cranial nerves IV. VI or VII are affected.
c. Autonomic neuropathy
- DM related autonomic neuropathy can involve multiple systems, including: the cardiovascular, GI, genitourinary, and metabolic systems
- It may also result in hypoglycemic unawareness due to reduction in counter regulatory hormone release.
References
Bezabeh ,M. ; Tesfaye,A.; Ergicho, B.; Erke, M.; Mengistu, S. and Bedane,A.; Desta, A.(2004). General Pathology. Jimma University, Gondar University Haramaya University, Dedub University.



|
|
|
|
دخلت غرفة فنسيت ماذا تريد من داخلها.. خبير يفسر الحالة
|
|
|
|
|
|
|
ثورة طبية.. ابتكار أصغر جهاز لتنظيم ضربات القلب في العالم
|
|
|
|
|
|
|
سماحة السيد الصافي يؤكد ضرورة تعريف المجتمعات بأهمية مبادئ أهل البيت (عليهم السلام) في إيجاد حلول للمشاكل الاجتماعية
|
|
|