
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 22-2-2016
Date: 22-2-2016
Date: 22-2-2016
|
Tuberculosis
Tuberculosis is a prototype example of granulomatous inflammation. Tuberculosis infects one third of world populations and kills about three million people yearly and it is the single most important infectious disease.
Etiology:
Mycobacterium tuberculosis and Mycobacterium bovis are the regular infecting rod shaped, acid fast and alcohol fast, strict aerobic, non-spore forming bacteria with a waxy coat. It has a slow generation time of 4-6 weeks to obtain a colony of mycobacterium tuberculosis. M. tuberculosis is transmitted by inhalation of infective droplets coughed or sneezed into the air by a patient with open tuberculosis, however, M. bovis is transmitted by milk from infected cows. Rarely, it transmits via breached skin surfaces and conjunctiva. M. Avium and M. intracellulare cause disseminated infection in 15%-24% of patients with AIDS.
Pathogenicity of the bacillus is related to its cell wall components. Pathogenicty of tuberculosis is attributed to its cell wall component.
1. Cord factor which is a cell wall glycolipid component is aviable on virulent strains
2. Lipoarabinomannan (LAM): It inhibits macrophage activation by interferonδ LAM induce macrophages to secrete TNF - α which causes fever, weight loss, and tissue damage and LAM also induce IL-10 which suppresses mycobacteria induced T-cell proliferation
3. Complement activated on the surface of mycobacteria may opsinize the organism and facilitate its uptake by macrophages complement receptor CR3 (mac-1 integrin) without triggering the respiratory burst necessary to kill the organisms.
4. M. Tuberculosis heat shock protein is similar to human heat shock protein and may have a role in autoimmune reactions induced by M. tuberculosis.
The bacillus resides in phagosome, which are not acidified in lysosomes. Inhibition of acidification has been associated with urase secreted by the mycobacteria.
Who are those more susceptible to develop tuberculosis?
- Race: North American Indians, black Africans and Asians are much more susceptible than others
- Age: Extremes of ages due to imperfect immune responses
- Immunologic and other host factors immunocompromized patients are more liable to develop tuberculosis. These include patients with steroid therapy or immunosuppressive drugs, HIV infection, diabetes mellitus, cirrhosis, malnutrition and damage of lung for example with silicosis etc.
Pathogenesis:
Primary infection: Primary phase of M. tuberculosis infection begins with inhalation of the mycobacteria most often in the lower segment of the lower and middle lobes and anterior segment of the lower lobe of the lung. First, the organisms are phagocytosed by alveolar macrophages and transported by these cells to hilar lymph nodes. Naïve macrophages are unable to kill the mycobacteria, thus they multiply and lyse these host cells, infect other macrophages and sometimes disseminate through blood to other parts of the lung and elsewhere in the body.
- After few weeks T-cell mediated immunity is demonstrable by PPD reaction first the CD4 T cells interaction with macrophages secrete interferon, which activate macrophages to kill intracellular mycobacteria through reactive nitrogen intermediates, including NO, NO2, HNO3.
- Second CD 8+ suppressor T-cells lyse macrophages infected with mycobacteria through a FAS -independent, granular dependent reaction and kill mycobacteria.
- Third CD4-CD8- (double negative) T cell lyse macrophages in a FAS dependant manner without killing mycobacteria. Lyses of these macrophages results in the formation of caseating granuloma and direct toxicity to the mycobacteria may contribute to the necrotic caseous centers.
The primary infection of sub-pleural lesion, the intervening macrophage reactions within accompanying lymphangitis and the hilar lymph nodes caseous lesions is called primary complex (often called a Ghon focus).
Hence, fate of primary complex include
i). T-cell mediated immune response induces hypersensitivity to the organisms and controls 95% of primary infection. This is associated with progressive fibrosis and calcification of persistent caseous debris. Moreover, most bacilli die but few remain viable for years until the person’s immune response fails.
However, if the infected person is immunologically immature, as in a young child or immunocompromized (eg. AIDS patients) the course of this primary infection is quite different. Such persons lack the capacity to coordinate integrated hypersensitivity and cell- mediated immune responses to the organism and thus often lack the capacity to contain the infection. Granulomas are poorly formed or not formed at all, and infection progresses at the primary site in the lung, the regional lymph nodes or at multiple sites of disseminations. This process produces progressive primary tuberculosis.
ii. Progressive primary tuberculous pneumonia: commonly seen in children less than five years of age but it ours in adults as well in those with suppressed or defective immunity.
iii. Subpleural focus may discharge bacilli or antigen into the pleural cavity resulting in the development of pleural effusion. It is common in adolescent infected with M. tuberculosis for the first time. Hilar or mediastinal groups of lymph nodes enlargement with caseous necrosis that may result in:
a. Obstruction of the bronchus by the enlarged lymph nodes leading to lobar collapse.
b. The caseous hilar lymph node may penetrate the bronchial wall and resulting in rupture of the wall with pouring of caseous materials into the bronchus hence, tuberculosis broncho-pneumonia ensues.
iv. The caseous materials may be disseminated to other parts of the body via blood streams.
Miliary tuberculosis
It refers to disseminated sites that produce multiple, small yellow nodular lesions in several organs. The term miliary emphasizes the resemblance of the lesion to millet seeds. The lungs, lymph nodes, kidneys, adrenals, bone marow, spleen, menings and liver are common sites for miliary lesions.
v. Seeding of the bacilli in lungs, bones, kidneys, fallopian tubes, bladder, epididimis etc, that may persist in and their subsequent reactivation produces destructive, necrotizing granulomatous disease, sometimes known as end organ tuberculosis.
Others sites of primary tuberculosis infection
i. Intestinal primary infection
The primary complex is similar to that of the lungs the initial site may be in the gum with lymphatic spread of bacilli to the cervical lymph nodes the commonest location for the primary lesion is the illocaecal region with local mesenteric node involvement.
ii. Lymph nodes
Tuberculous lymph adenitis is the most common type of extra pulmonary tuberculosis that frequently involves the cervical groups of lymph nodes with enlargement, and subsequent periadenitis followed by matting and eventual ulcerations if left untreated.
iii. Skin is also involved in various forms of tuberculosis
Post -primary (secondary) tuberculosis
Conventionally the term post-primary tuberculosis is used for lung infections occurring 5 years or more after the primary infection. If an adult acquires TB for the first time, it presents as post primary not Primary manifestation. The commonest sites for post primary tuberculosis are the posterior or apical segment of the upper lobe and the superior segment of the lower lobe and their predilection for the anatomy location is due to good ventilation. Hilar lymph node enlargement is not usually recorded. Hypersensitivity reaction is well-developed and it thus, restricts the granulomatous reactions locally. Post primary Tuberculosis is characterized by cavitary and fibrosing lesions. Pulmonary and bronchial arteries around caseous cavities are occluded by endarteritis obliterans where the wall of the artery may weaken resulting in aneurysm formation (mycotic aneurism) that may occasionally rupture and cause hemoptosis.
Post primary (20) tuberculosis in endemic countries occurs due to re-infection or reactivation of previously residing bacilli. In non-endemic (uncommon) countries, reactivation phenomenon is more important.
- Infected sputa may be swallowed resulting in tuberculous ulcer in the larynx or small intestine
- Secondary amyloidosis is a common complication of chronic tuberculosis. Certain tissues are relatively resistant to tuberculous infection, so it is rare to find tubercles in the heart, skeletal muscle, thyrord and pancreas.
M. tuberculosis and M. avium intracellulare lesions in AIDS
Mycobacteria infection in AIDS patients can take three forms depending on the degree of immunosuppression.
1. HIV infected individuals often have primary and secondary M. tuberculosis infection with the usual well-formed granulomas and acid fast my cobacteria are few in number and Often difficult to find under microscopy.
2. When HIV positive patient develop AIDS with moderate immunosuppression (less than 200 CD4+ heper T-cell /mm3) which is characterized by failure of helper T-cells to elaborate lymphokines and the relative increase in the number of CD 8+ cytotoxic T-cells may also cause macrophage destruction in the M. tuberculosis lesions. This results in less well-formed granulomas, and more frequently necrotic material that contain more abundant acid-fast organisms histologically.
Sputum is positive for acid-fast bacilli in 31%-82% of patients with AIDS. Extra pulmonary tuberculosis occurs in 70% of such patients involving lymph nodes, blood, CNS and bowel.
3. Opportunistic infection with M. avium- interacellurare occurs in severely immuno suppressed patients (less than 60 CD4+ cells /mm3. Most of these infections originate in the gastrointestinal tract. These infections are usually widely disseminated throughout the reticuloendothelial systems causing enlargement of involved lymph nodes, liver and spleen. The organisms are present in large numbers as many as 1010 organism per gram of tissue. Granulomas, lymphocytes and tissue destruction are rare.
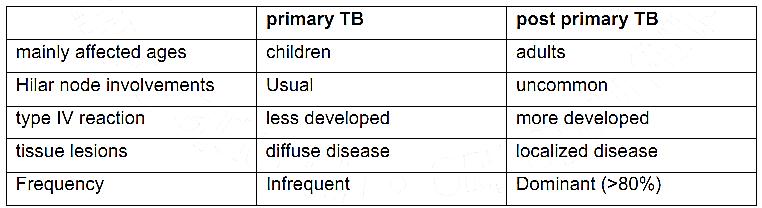
Differences between primary and post primary tuberculosis
Diagnosis of tuberculosis include:
Radiography
Culture
Zeihl Neelsen stain for Acid fast bacilli
Fine needle aspiration cytology
Exsional biopsy
References
Bezabeh ,M. ; Tesfaye,A.; Ergicho, B.; Erke, M.; Mengistu, S. and Bedane,A.; Desta, A.(2004). General Pathology. Jimma University, Gondar University Haramaya University, Dedub University.



|
|
|
|
دراسة يابانية لتقليل مخاطر أمراض المواليد منخفضي الوزن
|
|
|
|
|
|
|
اكتشاف أكبر مرجان في العالم قبالة سواحل جزر سليمان
|
|
|
|
|
|
|
المجمع العلمي ينظّم ندوة حوارية حول مفهوم العولمة الرقمية في بابل
|
|
|