
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 7-3-2016
Date: 9-3-2016
Date: 15-3-2016
|
Clostridium
Clostridia are 3-8 µm long, thick, Gram-positive, sporing rod bacteria that can only be cultured anaerobically. Their natural habitat is the soil. The pathogenicity of the disease-causing species in this genus is due to production of exotoxins and/or exoenzymes. The most frequent causative organism in anaerobic cellulitis and gas gangrene (clostridial myonecrosis) is C. perfrin- gens. Tetanus is caused by C. tetani. This pathogen produces the exotoxin te-tanospasmin, which blocks transmission of inhibitory CNS impulses to motor neurons. Botulism is a type of food poisoning caused by the neurotoxins of C. botulinum. These substances inhibit stimulus transmission to the motor end plates. Pseudomembranous colitis is caused by C. difficile, which produces an enterotoxin (A) and a cytotoxin (B). Diagnosis of clostridial infections requires identification of the pathogen (gas gangrene) and/or the toxins (tetanus, botulism, colitis). All clostridia are readily sensitive to penicillin G. Antitoxins are used in therapy of tetanus and botulism and hyperbaric O2 is used to treat gas gangrene. The most important preventive measure against tetanus is active vaccination with tetanus toxoid.
Occurrence. Clostridia are sporing bacteria that naturally inhabit the soil and the intestinal tracts of humans and animals. Many species are apathogenic saprophytes. Under certain conditions, several species cause gas gangrene, tetanus, botulism, and pseudomembranous colitis.
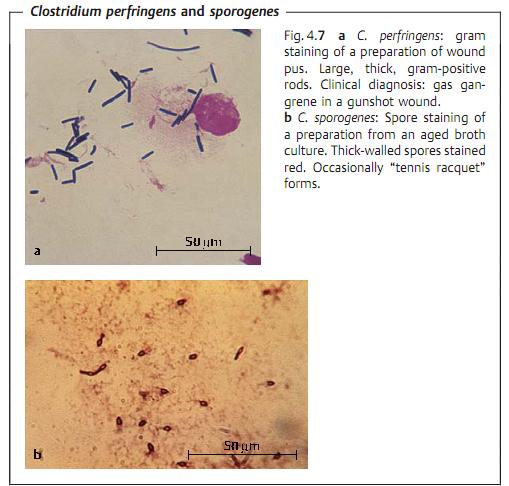
Morphology and culturing. All clostridia are large, Gram-positive rod bacteria about 1 µm thick and 3-8 µm in length (Fig. 4.7). Many cells in older cultures show a Gram-negative reaction. With the exception of C. perfringens, clostridia are flagellated. Clostridia sporulate. They are best cultured in an anaerobic atmosphere at 37 °C. C. perfringens colonies are convex, smooth, and surrounded by a hemolytic zone. Colonies of motile clostridia have an irregular, ragged edge.
The Pathogens That Cause Gas Gangrene (Clostridial Myonecrosis) and Anaerobic Cellulitis
Pathogen spectrum. The pathogens that cause these clinical pictures include Clostridium perfringens, C. novyi, C. septicum, and C. histolyticum. Species observed less frequently include C. sporogenes, C. sordellii, and C. bifermentans. The most frequent causative pathogen in gas gangrene is C. perfringens.
Toxins, enzymes. The toxins produced by invasive clostridia show necrotizing, hemolytic, and/or lethal activity. They also produce collagenases,proteinases, DNases, lecithinases, and hyaluronidase, all of which destroy tissue structures, resulting in accumulations of toxic metabolites.
Pathogenesis and clinical picture. Due to the ubiquitous presence of clostridia, they frequently contaminate open wounds, often together with other microorganisms. Detection of clostridia in a wound is therefore no indication of a clostridial infection. These infections develop when a low tissue redox potential makes anaerobe reproduction possible, resulting in tissue necrosis. Two such infections of differing severity are described below:
- Anaerobic cellulitis. Infection restricted to the fascial spaces that does not affect musculature. Gas formation in tissues causes a cracking, popping sensation under the skin known as crepitus. There is no toxemia.
- Gas gangrene (clostridial myonecrosis). An aggressive infection of the musculature with myonecrosis and toxemia. The incubation period varies from hours to a few days.
Diagnosis. The diagnostic procedure includes identification of the pathogens in relevant materials by means of microscopy and culturing. Identification of anaerobically grown cultures is based on morphological and physiological characteristics.
Therapy. Primary treatment is surgical, accompanied by antibiosis (penicillins, cephalosporins). Treatment with hyperbaric O2 in special centers has proved effective: patients breathe pure O2 through a tube or mask in a pressure chamber (3 atm = 303 kPa) several times during two-hour periods.
Epidemiology and prevention. True gas gangrene is now a rare condition. Timely operation of contaminated wounds is the main preventive measure.
Clostridium tetani (Tetanus)
Tetanus (lockjaw) is an acute clostridial disease, its clinical manifestations do not result directly from the invasive infection, but are rather caused by a strong neurotoxin.
Toxin. Tetanospasmin (an AB toxin, p. 16) consists of two polypeptide chains linked by a disulfide bridge. The heavy chain binds specifically to neuron receptors. The light chain is a zinc-metalloprotease that is responsible for proteolysis of components of the neuroexocytosis apparatus in the synapses of the anterior horns of the spinal cord. This stops transmission of inhibitory efferent impulses from the cerebellum to the motor end plates.
Pathogenesis and clinical picture. These ubiquitous pathogens invade tissues following injuries (Fig. 4.8a). Given anaerobic conditions, they proliferate and produce the toxin (see above), which reaches the anterior horns of the spinal cord or brain stem via retrograde axonal transport. The clinical picture resulting from the effects of the toxin is characterized by increased muscle tone and spasms induced by visual or acoustic stimuli. The cramps often begin in the facial musculature (risus sardonicus, Fig. 4.8b), then spread to neck and back muscles (opisthotonus). The patient remains lucid.
Diagnosis. The preferred method is toxin detection in wound material in an animal test (mouse) based either on neutralization or detection of the toxin gene with PCR. The pathogen is difficult to culture.
Therapy. Antitoxic therapy with immune sera is applied following a meticulous wound cleaning. The patient's musculature must also be relaxed with curare or similar agents.

Epidemiology and prophylaxis. Tetanus is now rare in developed countries due to widespread vaccination practice with incidence rates of approximately one case per million inhabitants per year. The frequency of occurrence is much higher in developing or underdeveloped countries. Worldwide, about 300 000 persons contract tetanus every year, with a lethality rate of approximately 50%. Thus, the importance of the active vaccination as a protective measure can hardly be overstated . A dose of Td should be administered once every 10 years to sustain protection . A booster shot is also required in case of severe injury if the patient's last inoculation was administered longer than five years before, and in case of minor injury longer than 10 years. Human tetanus immunoglobulin (250IU) must be administered to severely injured persons with insufficient vaccination protection or if the basic immunization history is uncertain.
Clostridium botulinum (Botulism)
Foodborne botulism is not an infection, but rather an intoxication, that is, the toxin is ingested with food. Infant botulism involves ingestion of spores and wound botulism results from infection of a wound.
Toxin. The very strong botulinum neurotoxin is a heat-labile protein. Seven toxigenic types are differentiated, each of which produces an immunologically distinct form of botulinum toxin. Types A, B, and E cause poisoning in humans. The toxin is a metalloprotease that catalyzes the proteolysis of components of the neuroexocytosis apparatus in the motor end plates, resulting in flaccid paralysis of the musculature.
Pathogenesis and clinical picture. Classic botulism results from eating spoiled foods in which the toxin has been produced under anaerobic conditions by C. botulinum. The toxin is absorbed in the gastrointestinal tract, and then transported to the peripheral nervous system in the bloodstream.
Within a matter of hours or days paralysis symptoms occur, especially in the nerves of the head. Frequent symptoms include seeing double, difficulty swallowing and speaking, constipation, and dry mucosa. Lethality rates range from 25-70%, depending on the amount of toxin ingested. Death usually results from respiratory paralysis. Wound botulism results from wound infection by C. botulinum and is very rare. Infant botulism, first described in 1976, results from ingestion of spores with food (e.g., honey). Probably due to the conditions prevailing in the intestines of infants up to the age of six months, the spores are able to proliferate there and produce the toxin. The lethality of infant botulism is low (<1%).
Diagnosis. Based on toxin detection by means of the mouse neutralization test.
Therapy. Urgent administration of a polyvalent antitoxin.
Epidemiology and prevention. Botulism is a rare disease. Exposure to the toxin is a food hygiene problem that can be avoided by taking appropriate precautions during food production. Aerosolized botulinum toxin has been used experimentally as a bioweapon.
Clostridium difficile (Pseudomembranous Colitis)
C. difficile occurs in the fecal flora of 1-4% of healthy adults and in 30-50% of children during the first year of life. The factors that lead to development of the disease are not known with certainty. Cases of pseudomembranous colitis are observed frequently under treatment with clindamycin, aminopenicillins, and cephalosporins (hence the designation antibiotic-associated colitis), but also occur in persons not taking antibiotics. Occasional outbreaks are seen in hospitals. The pathological mechanism is based on formation of two toxins. Toxin A is an enterotoxin that causes a dysfunction characterized by increased secretion of electrolytes and fluids. Toxin B is a cytotoxin that damages the mucosa of the colon.
The clinical course includes fever, diarrhea, and spasmodic abdominal pains. Coloscopy reveals edematous changes in the colon mucosa, which is also covered with yellowish-whitish matter. Laboratory diagnosis involves culturing the pathogen from patient stool and detection of the cytotoxin in bacteria-free stool filtrates on the basis of a cytopathic effect (CPE) observed in cell cultures, which CPE is then no longer observed after neutralization with an antiserum. Toxins A and B can also be detected with immunological test kits . A specific therapy is not required in many cases. Antibiotic treatment is indicated in severe cases. The agent of choice is currently metronidazole.



|
|
|
|
تفوقت في الاختبار على الجميع.. فاكهة "خارقة" في عالم التغذية
|
|
|
|
|
|
|
أمين عام أوبك: النفط الخام والغاز الطبيعي "هبة من الله"
|
|
|
|
|
|
|
قسم شؤون المعارف ينظم دورة عن آليات عمل الفهارس الفنية للموسوعات والكتب لملاكاته
|
|
|