
 النبات
النبات
 الحيوان
الحيوان
 الأحياء المجهرية
الأحياء المجهرية
 علم الأمراض
علم الأمراض
 التقانة الإحيائية
التقانة الإحيائية
 التقنية الحيوية المكروبية
التقنية الحيوية المكروبية
 التقنية الحياتية النانوية
التقنية الحياتية النانوية
 علم الأجنة
علم الأجنة
 الأحياء الجزيئي
الأحياء الجزيئي
 علم وظائف الأعضاء
علم وظائف الأعضاء
 الغدد
الغدد
 المضادات الحيوية
المضادات الحيوية|
Read More
Date: 28-12-2021
Date: 10-12-2021
Date: 5-1-2022
|
Jaundice
Jaundice (or, icterus) refers to the yellow color of skin, nail beds, and sclerae (whites of the eyes) caused by bilirubin deposition, secondary to increased bilirubin levels in the blood (hyperbilirubinemia) as shown in Figure1. Although not a disease, jaundice is usually a symptom of an underlying disorder. [Note: Blood bilirubin levels are normally ≤1 mg/dl. Jaundice is seen at 2–3 mg/dl.]
Figure 1: Jaundiced patient with the sclerae of his eyes appearing yellow.
1. Types: Jaundice can be classified into three major types described below. However, in clinical practice, jaundice is often more complex than indicated in this simple classification. For example, the accumulation of bilirubin may be a result of defects at more than one step in its metabolism.
a. Hemolytic (prehepatic): The liver has the capacity to conjugate and excrete >3,000 mg of bilirubin/day, whereas the normal production of bilirubin is only 300 mg/day. This excess capacity allows the liver to respond to increased heme degradation with a corresponding increase in conjugation and secretion of CB. However, extensive hemolysis (for example, in patients with sickle cell anemia or deficiency of pyruvate kinase or glucose 6-phosphate dehydrogenase) may produce bilirubin faster than it can be conjugated. UCB levels in the blood become elevated (unconjugated hyperbilirubinemia), causing jaundice (Fig. 2A). [Note: With hemolysis, more CB is made and excreted into the bile, the amount of urobilinogen entering the enterohepatic circulation is increased, and urinary urobilinogen is increased.]
Figure 2: Alterations in the metabolism of heme. A. Hemolytic jaundice. B. Neonatal jaundice. = conjugated bilirubin; = bilirubin; = urobilinogen; = stercobilin; UDP = uridine diphosphate.
b. Hepatocellular (hepatic): Damage to liver cells (for example, in patients with cirrhosis or hepatitis) can cause unconjugated hyperbilirubinemia as a result of decreased conjugation. Urobilinogen is increased in the urine because hepatic damage decreases the enterohepatic circulation of this compound, allowing more to enter the blood, from which it is filtered into the urine. The urine consequently darkens, whereas stools may be a pale, clay color. Plasma levels of alanine and aspartate transaminases (ALT and AST, respectively) are elevated. If CB is made but is not efficiently secreted from the liver into bile (intrahepatic cholestasis), it can leak into the blood (regurgitation), causing a conjugated hyperbilirubinemia.
c. Obstructive (posthepatic): In this instance, jaundice is not caused by overproduction of bilirubin or decreased conjugation but, instead, results from obstruction of the common bile duct (extrahepatic cholestasis). For example, the presence of a tumor or bile stones may block the duct, preventing passage of CB into the intestine. Patients with obstructive jaundice experience GI pain and nausea and produce stools that are a pale, clay color. The CB regurgitates into the blood (conjugated hyperbilirubinemia). The CB is eventually excreted in the urine (which darkens over time) and is referred to as urinary bilirubin. Urinary urobilinogen is absent.
2. Jaundice in newborns: Most newborn infants (60% of full term and 80% of preterm) show a rise in UCB in the first postnatal week (and a transient, physiologic jaundice) because the activity of hepatic bilirubin UGT is low at birth (it reaches adult levels in about 4 weeks), as shown in Figures 2B and 3. Elevated UCB, in excess of the binding capacity of albumin (20–25 mg/dl), can diffuse into the basal ganglia, causing toxic encephalopathy (kernicterus) and a pathologic jaundice. Therefore, newborns with significantly elevated bilirubin levels are treated with blue fluorescent light (phototherapy), as shown in Figure 4, which converts bilirubin to more polar and, therefore, watersoluble isomers. These photoisomers can be excreted into the bile without conjugation to glucuronic acid. [Note: Because of solubility differences, only UCB crosses the blood–brain barrier, and only CB appears in urine.]
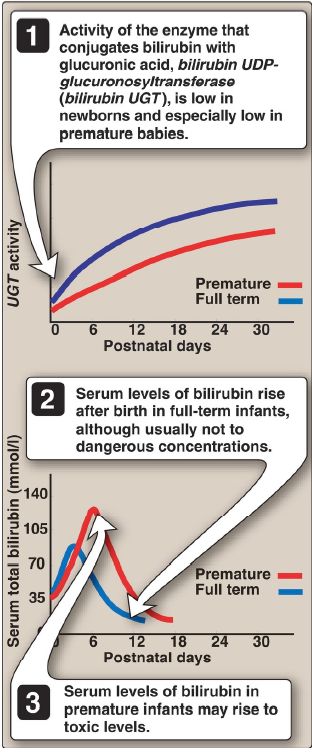
Figure 3: Neonatal jaundice. UDP = uridine diphosphate.

Figure 4: Phototherapy in neonatal jaundice.
3. Bilirubin measurement: Bilirubin is commonly measured by the van den Bergh reaction, in which diazotized sulfanilic acid reacts with bilirubin to form red azodipyrroles that are measured colorimetrically. In aqueous solution, the water-soluble CB reacts rapidly with the reagent (within 1 minute) and is said to be direct reacting. The UCB, which is much less soluble in aqueous solution, reacts more slowly. However, when the reaction is carried out in methanol, both CB and UCB are soluble and react with the reagent, providing the total bilirubin value. The indirectreacting bilirubin, which corresponds to the UCB, is obtained by subtracting the direct-reacting bilirubin from the total bilirubin. [Note: In normal plasma, only ~4% of the total bilirubin is conjugated, or direct reacting, because most is secreted into bile.]



|
|
|
|
"عادة ليلية" قد تكون المفتاح للوقاية من الخرف
|
|
|
|
|
|
|
ممتص الصدمات: طريقة عمله وأهميته وأبرز علامات تلفه
|
|
|
|
|
|
|
الأمين العام للعتبة العسكرية المقدسة يستقبل شيوخ ووجهاء عشيرة البو بدري في مدينة سامراء
|
|
|