

النبات

مواضيع عامة في علم النبات

الجذور - السيقان - الأوراق

النباتات الوعائية واللاوعائية

البذور (مغطاة البذور - عاريات البذور)

الطحالب

النباتات الطبية


الحيوان

مواضيع عامة في علم الحيوان

علم التشريح

التنوع الإحيائي

البايلوجيا الخلوية


الأحياء المجهرية

البكتيريا

الفطريات

الطفيليات

الفايروسات


علم الأمراض

الاورام

الامراض الوراثية

الامراض المناعية

الامراض المدارية

اضطرابات الدورة الدموية

مواضيع عامة في علم الامراض

الحشرات


التقانة الإحيائية

مواضيع عامة في التقانة الإحيائية


التقنية الحيوية المكروبية

التقنية الحيوية والميكروبات

الفعاليات الحيوية

وراثة الاحياء المجهرية

تصنيف الاحياء المجهرية

الاحياء المجهرية في الطبيعة

أيض الاجهاد

التقنية الحيوية والبيئة

التقنية الحيوية والطب

التقنية الحيوية والزراعة

التقنية الحيوية والصناعة

التقنية الحيوية والطاقة

البحار والطحالب الصغيرة

عزل البروتين

هندسة الجينات


التقنية الحياتية النانوية

مفاهيم التقنية الحيوية النانوية

التراكيب النانوية والمجاهر المستخدمة في رؤيتها

تصنيع وتخليق المواد النانوية

تطبيقات التقنية النانوية والحيوية النانوية

الرقائق والمتحسسات الحيوية

المصفوفات المجهرية وحاسوب الدنا

اللقاحات

البيئة والتلوث


علم الأجنة

اعضاء التكاثر وتشكل الاعراس

الاخصاب

التشطر

العصيبة وتشكل الجسيدات

تشكل اللواحق الجنينية

تكون المعيدة وظهور الطبقات الجنينية

مقدمة لعلم الاجنة


الأحياء الجزيئي

مواضيع عامة في الاحياء الجزيئي


علم وظائف الأعضاء


الغدد

مواضيع عامة في الغدد

الغدد الصم و هرموناتها

الجسم تحت السريري

الغدة النخامية

الغدة الكظرية

الغدة التناسلية

الغدة الدرقية والجار الدرقية

الغدة البنكرياسية

الغدة الصنوبرية

مواضيع عامة في علم وظائف الاعضاء

الخلية الحيوانية

الجهاز العصبي

أعضاء الحس

الجهاز العضلي

السوائل الجسمية

الجهاز الدوري والليمف

الجهاز التنفسي

الجهاز الهضمي

الجهاز البولي


المضادات الميكروبية

مواضيع عامة في المضادات الميكروبية

مضادات البكتيريا

مضادات الفطريات

مضادات الطفيليات

مضادات الفايروسات

علم الخلية

الوراثة

الأحياء العامة

المناعة

التحليلات المرضية

الكيمياء الحيوية

مواضيع متنوعة أخرى

الانزيمات
ENTAMOEBA
المؤلف:
Warren Levinson
المصدر:
Review of Medical Microbiology and Immunology
الجزء والصفحة:
13th Edition , p920-925
2025-01-01
1579
Diseases
Entamoeba histolytica causes amebic dysentery and liver abscess.
Important Properties
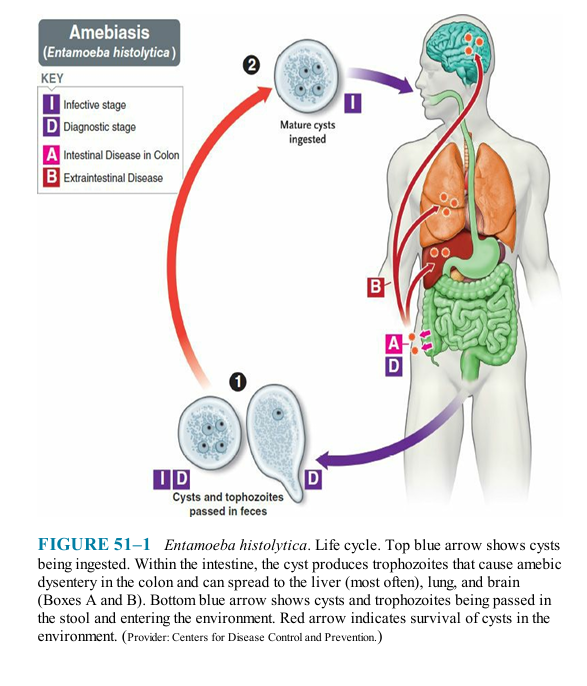
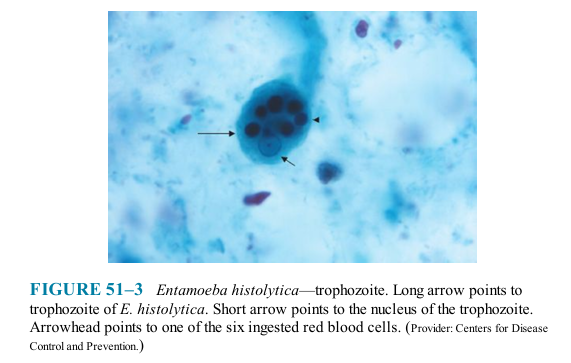
The life cycle of E. histolytica is shown in Figure 51-1. The life cycle has two stages: the motile ameba (trophozoite) and the nonmotile cyst (Figures 51-2A and B, 51-3, and 51-4). The trophozoite is found within the intestinal and extraintestinal lesions and in diarrheal stools. The cyst predominates in non-diarrheal stools. These cysts are not highly resistant and are readily killed by boiling but not by chlorination of water supplies. They are removed by filtration of water.
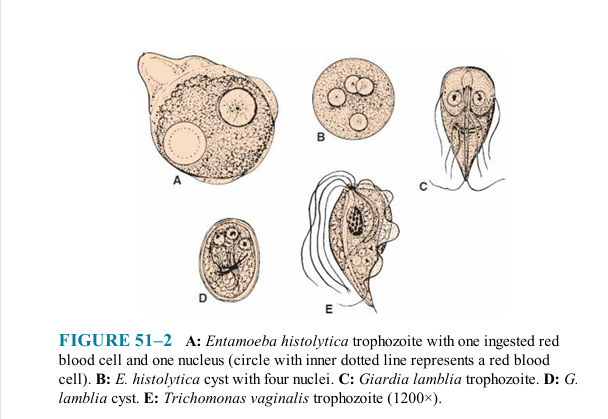
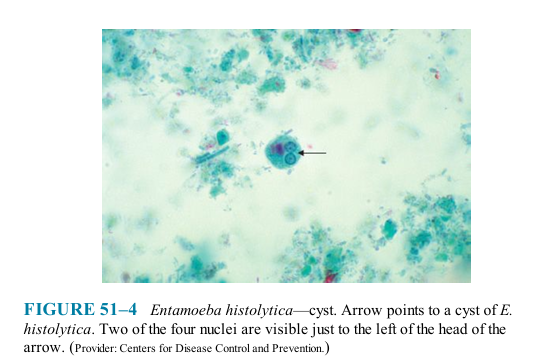
The cyst has four nuclei, an important diagnostic criterion. Upon excystation in the intestinal tract, an ameba with four nuclei emerges and then divides to form eight trophozoites. The mature trophozoite has a single nucleus with an even lining of peripheral chromatin and a prominent central nucleolus (karyosome).
Antibodies are formed against trophozoite antigens in invasive amebiasis, but they are not protective; previous infection does not prevent reinfection. The antibodies are useful, however, for serologic diagnosis.
Pathogenesis & Epidemiology
The organism is acquired by ingestion of cysts that are transmitted primarily by the fecal-oral route in contaminated food and water. Anal-oral transmission (e.g., among male homosexuals) also occurs. There is no animal reservoir. The ingested cysts differentiate into trophozoites in the ileum but tend to colonize the cecum and colon.
The trophozoites invade the colonic epithelium and secrete enzymes that cause localized necrosis. Little inflammation occurs at the site. As the lesion reaches the muscularis layer, a typical "flask-shaped" ulcer forms that can undermine and destroy large areas of the intestinal epithelium . Progression into the submucosa leads to invasion of the portal circulation by the trophozoites. By far the most frequent site of systemic disease is the liver, where abscesses containing Infection by E. histolytica is found worldwide but occurs most frequently in tropical countries, especially in areas with poor sanitation. About 1% to 2% of people in the United States are affected. Infection is common in men who have sex with men.
Clinical Findings
Acute intestinal amebiasis presents as dysentery (i.e., bloody, mucus-containing diarrhea) accompanied by lower abdominal discomfort, flatulence, and tenesmus. Chronic amebiasis with low-grade symptoms such as occasional diarrhea, weight loss, and fatigue also occurs. Roughly 90% of those infected have asymptomatic infections, but they may be carriers, whose feces contain cysts that can be transmitted to others. In some patients, a granulomatous lesion called an ameboma may form in the cecal or rectosigmoid areas of the colon. These lesions can resemble an adenocarcinoma of the colon and must be distinguished from them.
Amebic abscess of the liver is characterized by right-upper-quadrant pain, weight loss, fever, and a tender, enlarged liver. Right-lobe abscesses can penetrate the diaphragm and cause lung disease. Most cases of amebic liver abscess occur in patients who have not had overt intestinal amebiasis.
Laboratory Diagnosis
Diagnosis of intestinal amebiasis rests on finding either trophozoites in diarrheal stools or cysts in formed stools (Figures 51-3 and 51-4). Diarrheal stools should be examined within 1 hour of collection to see the ameboid motility of the trophozoite. Trophozoites characteristically contain ingested red blood cells. The most common error is to mistake fecal leukocytes for trophozoites. Because cysts are passed intermittently, at least three specimens should be examined. The O&P test is insensitive and false negatives commonly occur. Also, about half of the patients with extraintestinal amebiasis have negative stool examinations.
E. histolytica can be distinguished from other amebas by two major criteria: (1) The first is the nature of the nucleus of the trophozoite. The E. histolytica nucleus has a small central nucleolus and fine chromatin granules along the border of the nuclear membrane. The nuclei of other amebas are quite different. (2) The second is cyst size and number of its nuclei. Mature cysts of E. histolytica are smaller than those of Entamoeba coli and contain four nuclei, whereas E. coli cysts have eight nuclei.
The trophozoites of Entamoeba dispar, a nonpathogenic species of Entamoeba, are morphologically indistinguishable from those of E. histolytica; therefore, a person who has trophozoites in the stool is only treated if symptoms warrant it. Two tests are highly specific for E. histolytica in the stool: one detects E. histolytica antigen, and the other detects nucleic acids of the organism in a polymerase chain reaction (PCR)-based assay.
A complete examination for cysts includes a wet mount in saline, an iodine- stained wet mount, and a fixed, trichrome-stained preparation, each of which brings out different aspects of cyst morphology. These preparations are also helpful in distinguishing amebic from bacillary dysentery. In the latter, many inflammatory cells such as polymorphonuclear leukocytes are seen, whereas in amebic dysentery, they are not.
Serologic testing is useful for the diagnosis of invasive amebiasis. The indirect hemagglutination test is usually positive in patients with invasive disease but is frequently negative in asymptomatic individuals who are passing cysts.
Treatment
The treatment of choice for symptomatic intestinal amebiasis or hepatic abscesses is metronidazole (Flagyl) or tinidazole. Hepatic abscesses need not be drained. Asymptomatic cyst carriers should be treated with iodoquinol or paromomycin.
 الاكثر قراءة في الطفيليات
الاكثر قراءة في الطفيليات
 اخر الاخبار
اخر الاخبار
اخبار العتبة العباسية المقدسة

الآخبار الصحية















 قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة
قسم الشؤون الفكرية يصدر كتاباً يوثق تاريخ السدانة في العتبة العباسية المقدسة "المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة
"المهمة".. إصدار قصصي يوثّق القصص الفائزة في مسابقة فتوى الدفاع المقدسة للقصة القصيرة (نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)
(نوافذ).. إصدار أدبي يوثق القصص الفائزة في مسابقة الإمام العسكري (عليه السلام)


















